 By Brian Miller
By Brian Miller
According to the Federal Bureau of Investigation (FBI), a mass murder occurs when at least four people are murdered, not including the shooter, over a relatively short period of time during a single incident. Over the last 30 years, the United States has seen a significant increase in mass shootings, which are becoming more frequent and more deadly.
Seemingly every time a mass shooting occurs, whether it’s at a synagogue in Pittsburgh or a nightclub in Orlando, the anti-gun media and politicians have a knee-jerk response – they blame the tragedy solely on the tool used, namely firearms, and focus all of their proposed “solutions” on more laws, ignoring that the murderer already broke numerous laws when they committed their atrocity.
Facts matter when addressing such an emotionally charged topic, and more gun control legislation has shown that law-abiding Americans who own guns are not the problem. Consider the following: The more gun control laws that are passed, the more mass murders have occurred.
Whether or not this is correlation or causation is debatable. What is not debatable is that this sick phenomenon of mass murderers targeting “gun-free zones,” where they know civilian carry isn’t available to law-abiding Americans, is happening. According to the Crime Prevention Research Center, 97.8 percent of public shootings occur in “gun-free zones” – and “gun-free zones” are the epitome of the core philosophical tenant of gun control, that laws are all the defense one needs against violence.
Therefore, when the media and politicians focus their ire on guns, specifically what types of guns are used, such as AR-styles, carbines, semi-automatics, and “high capacity” handguns, in the wake of such tragedies the American public are being intentionally drawn into an emotionally charged debate about legal gun ownership (irrespective of whether the murderer’s gun was legally or illegally obtained). This debate leads them away from the elephant in the room and one of the real issues behind mass shootings – mental health and prescription drugs.
Ignoring what’s going on in the heads of these psychopaths not only allows mass shootings to continue, it leads to misguided gun control laws that violate the Second Amendment and negate the rights of law-abiding U.S. citizens. As Jeff Snyder put it in The Washington Times:
“But to ban guns because criminals use them is to tell the innocent and law-abiding that their rights and liberties depend not on their own conduct, but on the conduct of the guilty and the lawless, and that the law will permit them to have only such rights and liberties as the lawless will allow.”
Violence, especially random violence, is a complex manifestation of various thoughts, feelings, and external factors. When a multivariate analysis of these factors is conducted, it becomes apparent that it’s not just mental health issues that are leading to such an increase. There may be an underlying substance which plays a role in a high percentage of these violent acts – the use of prescription antidepressants, specifically selective serotonin reuptake inhibitors, or SSRIs.
At first glance, it makes sense that those involved in mass shootings may be taking antidepressants, as they’re clearly suffering from some sort of mental health issue. But the issue with SSRIs runs much deeper than just a random mental health break. These drugs are a prescription for violent crimes, and that’s a story the anti-gun media and politicians don’t want to talk about.
History of Antidepressant Use in the U.S.
 To understand the rise in antidepressant use, one must first understand depression. Everyone, no matter how great their life, has periods of sadness, times when they feel down or low. This is especially true when faced with hardships or going through things like a divorce, the loss of a job, or the death of a parent.
To understand the rise in antidepressant use, one must first understand depression. Everyone, no matter how great their life, has periods of sadness, times when they feel down or low. This is especially true when faced with hardships or going through things like a divorce, the loss of a job, or the death of a parent.
This is not clinical depression. Clinical depression is a serious mental disorder that impacts how a person functions on a daily basis. Depression makes it hard to get out of bed. It makes it hard to go to work. It makes it hard to take a shower or answer the phone. It stops a person from functioning on the basic levels.
Understanding Depression
According to the Diagnostic and Statistical Manual of Mental Disorders, commonly referred to as the DSM-5, to be considered clinically depressed, a patient must experience five of the following symptoms most of the day, every day, for at least two weeks. What’s more, these symptoms must be so severe, they interfere with normal functioning:
- Sadness
- Anxiety
- Feeling hopeless
- Feeling worthless
- Feeling helpless
- Feeling “empty”
- Feeling guilty
- Irritable
- Fatigue
- Lack of energy
- Loss of interest in hobbies
- Slow talking and moving
- Restlessness
- Trouble concentrating
- Abnormal sleep patterns, whether sleeping too much or not enough
- Abnormal weight changes, either eating too much or having no appetite
- Thoughts of death or suicide
Depression is a serious, and sometimes life-threatening, illness. But in the modern world, it’s highly over-diagnosed. A study published in Psychotherapy and Psychosomatics looked at 5,639 patients in the U.S. who were diagnosed with depression by their clinician and compared their symptoms to the DSM criteria for clinical depression. Of these patients, only 38.4 percent met the criteria, even though the majority of the 5,639 patients were prescribed depression medication.
Today, with the way antidepressants are prescribed, nearly one in four Americans will meet the criteria to be diagnosed with depression within their lifetime, and will be prescribed medications that interfere with how their brain functions.
The Rise of Antidepressants
In the 1950s, the first generation of antidepressants hit the market. The introductory class of antidepressants to gain Food and Drug Administration (FDA) approval were monoamine oxidase inhibitors, known as MAOIs. Although highly effective, MAOIs can cause extremely high blood pressure when paired with certain foods or medications, and therefore require diet restrictions. Because of these restrictions, they’re rarely used today to treat depression except in cases where other treatments fail.
By the late 1950s, a new class of antidepressants became available – tricyclic antidepressants. Tricyclic antidepressants are also highly effective for treating depression, but are prone to side effects. Even so, this class of antidepressants remained the go-to depression treatment for years. Other drugs were tested for depression treatment, but they hadn’t proved more effective than tricyclic and MAOI antidepressants, especially for severe depression.
Fast forward to the 1980s. America’s tranquilizer dependence was becoming problematic. Quaaludes were heavily over-prescribed for anxiety, resulting in overdose deaths, as well as an increase in deaths from vehicle accidents. The Feds stepped in and in 1984, classified Quaaludes as a Schedule 1 drug, making them illegal to sell, buy, and use.
Valium, a benzodiazepine prescribed for anxiety, was also extremely popular, and was the most prescribed medication in the U.S. from 1969 through 1982. In 1978, the year the medication peaked, more than 2.3 billion pills were sold in the U.S. But Valium was highly addictive and it was believed that a serotonergic medication was a better option to fill the void that was left when Quaaludes were outlawed.
In 1987, Prozac, the first SSRI, was released for depression. Along with it came the idea that depression could be the underlying cause of anxiety. The idea took off, as did the sales of Prozac, and within a few years, it overtook the antidepressant market. Soon, other SSRIs followed.
Along with these SSRIs came direct-to-consumer advertising, which became legal in 1985. By the mid-1990s, the FDA regulations became looser and direct-to-consumer ads exploded into the market. Prozac and other medications showed Americans through glossy advertisements that unhappiness, stress, and anxiety could be treated with a pill.
Instead of doctors recommending a specific medication, patients started coming in, requesting a medication they saw in a magazine or on television.
SSRI sales skyrocketed.
By 2010, 11 percent of Americans over the age of 12 were prescribed an antidepressant, making it the third most prescribed medication, topped only by nonsteroidal anti-inflammatory drugs (NSAIDs) like ibuprofen and naproxen. When looked at over time, there has been a 400-percent increase in antidepressant use from 1988 through 2008.
SSRIs 101: What You Should Know
 Selective serotonin reuptake inhibitors, a class of drugs commonly referred to as SSRIs, are the most prescribed antidepressant in the United States. These second-generation antidepressants are marketed to doctors and patients as safe and effective, with relatively minimal side effects. SSRIs are designated to treat mild to moderate depression, as well as anxiety, obsessive compulsive disorder, and bulimia nervosa.
Selective serotonin reuptake inhibitors, a class of drugs commonly referred to as SSRIs, are the most prescribed antidepressant in the United States. These second-generation antidepressants are marketed to doctors and patients as safe and effective, with relatively minimal side effects. SSRIs are designated to treat mild to moderate depression, as well as anxiety, obsessive compulsive disorder, and bulimia nervosa.
How do SSRIs work?
SSRIs work to increase the amount of serotonin in the brain. A neurotransmitter that helps neurons communicate, serotonin is associated with many different body functions, but is best known for its influence on mood. Sometimes called “the happy chemical,” serotonin plays a role in a person’s happiness and general feelings of wellbeing.
Low levels of serotonin are linked to depression, although the relationship is not clear. Research has not determined if the low neurotransmitter level causes depression or if depression causes the level of serotonin to drop. It should also be noted that a large amount of serotonin, up to 90 percent, is produced in the gut and may be influenced by what a person eats and drinks.
SSRI medication does exactly what its name says. When two neurons communicate, one releases neurotransmitters, which causes the other neuron to react in a certain way. Because this is constantly going on, these chemicals are always present in the brain. To keep the brain’s chemical balance correct, neurons regulate the amount of neurotransmitters released by a process called reuptake, which involves the reabsorption of the chemical by a neuron.
For instance, if there’s a high level of serotonin, the neuron knows to release less through reuptake, keeping the level balanced. If levels of the neurotransmitter are low, reuptake tells the neurons to release more.
SSRIs inhibit the reuptake of serotonin, causing neurons to release more of the neurotransmitter, therefore increasing the amount of the chemical found in the brain.
The Food and Drug Administration (FDA) has approved a variety of SSRIs, including:
- Citalopram (Celexa)
- Escitalopram (Lexapro)
- Fluoxetine (Prozac)
- Paroxetine (Paxil and Pexeva)
- Sertraline (Zoloft)
- Vilazodone (Viibryd)
When it comes to effectiveness, SSRIs don’t appear to have an influence on those with moderate to severe depression, with virtually no improvement seen when comparing SSRI use to placebos. Instead of a popular drug with a high efficiency, modern SSRIs have become popular based on an effective marketing campaign and little more.
Too Much of a Good Thing: Serotonin Syndrome
Sometimes serotonin levels become too high, causing Serotonin Syndrome. A potentially life-threatening disease, it occurs when serotonin levels in the brain increase to a toxic level, often caused by too much medication or taking two serotonin-increasing medications that use different mechanisms to increase the neurotransmitter.
Along with physical symptoms of excessive nerve activity, such as dilated pupils, elevated heart rate, and high blood pressure, those with the syndrome may also experience:
- Agitation
- Restlessness
- Confusion
- Anxiety
- Disorientation
- Excitement
The Connection Between SSRIs and Violence
 Regardless if depression is overdiagnosed and America has a habit of over-prescribing mind-altering medications, there’s little doubt that SSRIs have a risk of increasing violence in patients, even in patients who have no previous history of violence or aggression before taking the medication.
Regardless if depression is overdiagnosed and America has a habit of over-prescribing mind-altering medications, there’s little doubt that SSRIs have a risk of increasing violence in patients, even in patients who have no previous history of violence or aggression before taking the medication.
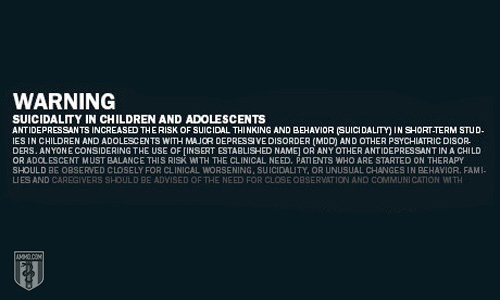
This risk of violent behavior, both to the individual taking the medication and those around them, is so significant, it has led to the FDA mandating a black box warning on all SSRI medications. These black box warnings are designed to provide information and draw attention to the fact that the medication has serious and life-threatening risks.
As of 2004, all antidepressants in the U.S. are labeled:
“Anxiety, agitation, panic attacks, insomnia, irritability, hostility, aggressiveness, impulsivity, akathisia, hypomania, and mania have been reported in adult and pediatric patients being treated with antidepressants for major depressive disorder as well as for indications, both psychiatric and nonpsychiatric.”
SSRIs Can Increase the Risk of Suicide
In one study published in the American Journal of Psychiatry, patients suffering from depression, but free of serious suicidal ideation, were given fluoxetine. Within two to seven weeks of starting the medication, six patients developed an intense, preoccupation with violent suicide. Although all were immediately taken off the medication, this preoccupation persisted from three days to three months, depending on the case. In all six cases, the patient had never experienced such a severe level of depression or troubled state of mind before or with other psychotropic prescriptions.
According to the Centers for Disease Control and Prevention Surveillance for Violent Deaths, in 2013, 35.3 percent of those who committed suicide tested positive for antidepressants at the time of their death.
The risk of SSRIs and suicide is most prevalent in patients under the age of 25. It’s also more likely to occur shortly after starting the medication, after a dosage increase, or after a patient stops taking the medication.
SSRIs Can Increase the Risk of Violence Against Others
Some of the side effects caused by SSRIs can increase the risk of violence against others. Perhaps the most risky, emotional blunting (or detachment) has been linked to SSRI use and many people who’ve taken the drugs report “not feeling” or “not caring” about anything. There’s also been an established causal relationship between SSRI use and psychosis and hallucinations, both of which are known to increase the risk of violence in individuals.
According to a review of the FDA’s database, 484 drugs were identified as triggers to serious adverse events significant enough to warrant a case study during the five-year period from 2004 through 2009. Of these 484 medications, 31 were identified to have a “disproportionate” association with violence. These 31 drugs make up 78.8 percent of all cases of violence toward others in the FDA’s database and included multiple psychotropic medications:
- 11 antidepressants
- 6 hypnotic/sedatives
- 3 ADHD medications
- 1 smoking cessation drug
Researchers concluded that violence against others was a “genuine and serious adverse drug event” and that of the 484 medications, the drugs that were most consistently and strongly associated with violence were the smoking cessation medication, varenicline (Chantix), and SSRIs.
The list includes five SSRI antidepressants:
- Fluoxetine: Prozac increased aggressive behavior 10.9 times
- Paroxetine: Paxil increased violent behavior 10.3 times
- Fluvoxamine: Luvox increased violent behavior 8.4 times
- Venlafaxine: Effexor increased violent behavior 8.3 times
- Desvenlafaxine: Pristiq increased violent behavior 7.9 times
While a surprise to the American public, this shouldn’t have been a surprise to the drug companies. During the clinical trials for paroxetine, hostility, which was the term to include homicidal idealization and aggression, presented in 60 of the 9,219 participants (.65 percent). Hostile acts were documented both while taking the medication and after tapering off. Children with obsessive-compulsive disorder (OCD) taking the medication were the most at risk for becoming hostile, with a 17-times higher probability than the rest of those in the clinical study.
In a Swedish study published in PLoS, researchers looked at information on over 850,000 patients prescribed SSRIs in the Swedish Prescribed Drug Register, which is a national database of all dispensed medications. They then compared the violent crimes committed during a three-year period and compared it to violent crimes committed by the same individuals when not taking the medications. When age was taken into effect, a significant association was apparent between violent crime convictions and SSRI use in patients between the ages of 15 and 24.
In one 2001 case, Cory Baadsgaard, a 16-year-old who attended Wahluke High School in Washington, was first prescribed Paxil, which caused hallucinations, and then was switched to Effexor. He started at a 40 mg dosage that, over the course of three weeks, increased to 300 mg. On the first day of that high dose, he woke with a headache and returned to bed. He then got up, took a rifle to his high school, and held 23 classmates hostage.
Baadsgaard’s testimony claims he has no recollection of the event, or of his principal convincing him to put the gun down and release the hostages.
In 2002, the BBC aired the documentary Panorama, which focused on paroxetine. The producers received 1,374 emails from viewers, the majority of whom told stories of violence or self-harm while taking the medication, particularly when starting and when increasing the dosage.
What’s more, in 2009, after investigating the connection between SSRIs and violence, the Japanese Ministry of Health, Labor, and Welfare revised the label warnings on these drugs to read: “There are cases where we cannot rule out a causal relationship [of hostility, anxiety, and sudden acts of violence] with the medication.”
Connection Between SSRI and Murder
 In most cases, the vast majority of people who suffer from mental illness are nonviolent. Even those who self-harm are highly unlikely to hurt others. In fact, these individuals are more likely to become victims of violent crimes than the general public.
In most cases, the vast majority of people who suffer from mental illness are nonviolent. Even those who self-harm are highly unlikely to hurt others. In fact, these individuals are more likely to become victims of violent crimes than the general public.
Yet after each mass shooting tragedy, the media fills with psychiatrists who say that the individual didn’t seek the help they needed and that with the proper treatment, the tragedy may have been prevented. But research doesn’t support that philosophy.
In fact, depression in particular doesn’t lead to violence, yet since the increase in SSRI antidepressants being widely prescribed, the rise in mass shootings has increased right along with it. And evidence shows that many mass shooters were either taking or had recently taken SSRIs.
Here are just some examples:
- 1989: Joseph T. Wesbecker walked into his former employer Standard Gravure Corp and shot 20 workers, killing nine. He had been taking Prozac for a month. This shooting led to a landmark case, where the survivors sued the makers of Prozac, Eli Lilly. Wesbecker used a semiautomatic Chinese AK-47-style firearm, a 9mm pistol, and a .38 Special snubnose revolver – all of which he purchased legally, passing his background check.
- 1995: Jarred Viktor was 15 when he was prescribed Paxil. Ten days after starting it, Viktor stabbed his grandmother 61 times.
- 1996: At 18, Kurt Danysh murdered his father just 17 days after being prescribed Prozac by his family doctor, who failed to do even one psychological test. During his police confession, Danysh told police the medication made him feel odd, “I just act differently. I don’t have the energy or personality I used to. I spend half the time in a trance.”
- 1997: Luke Woodham stabbed his mother, then traveled to Pearl High School, where he was enrolled, using a .30-30 to shoot two students and wound six others; he was stopped by his assistant principal (aka a good guy with a gun) who used his own .45 ACP handgun to force Woodham’s surrender.
- 1998: 15-year-old Kip Kinkel shot both of his parents, then carried a 9mm handgun, .22 rifle, and a .22 pistol to his Thurston High School, where he murdered two classmates and injured 22 more, all while taking Prozac.
- 1999: Eric Harris, 17, with Dylan Klebold, killed 12 students, one teacher, himself, and wounded 23 others during the Columbine school shooting; he had been prescribed Zoloft and then Luvox before he used a 12 gauge shotgun received through a straw purchaser and a 9mm TEC-DC9.
- 2001: Christopher Pittman, a 12-year-old, was prescribed Zoloft, which caused him to become agitated, jittery, and experience tactile hallucinations; Pittman told psychiatrist Dr. Lanette Atkins that he heard voices telling him, “Kill, kill, do it, do it.” He took a .410 shotgun and shot his grandparents, then burned their house down.
- 2001: Andrea Yates drowned all five of her children. She was taking Effexor and was suffering from delusions about satanic possession. The murder of her children led Effexor to list homicidal thoughts in the medication’s side effects. Although it’s a rare side effect, manifesting in one in 1,000 patients, over 19 million prescriptions were written and filled in 2005. That’s an estimated 19,000 people suffering from homicidal thoughts because of the medication.
- 2005: 16-year-old Jeff Weise was taking 60 mg/day of Prozac, the highest dosage for adults, when he shot his grandfather, his grandfather’s girlfriend, murdered 10 students at Red Lake, Minnesota, and wounded 12 more, before shooting himself. He was armed with a .40 caliber pistol, .22 pistol, and a 12 gauge shotgun.
- 2008: Steven Kazmierczak was prescribed Prozac, Xanax, and Ambien, a sleeping medication, three weeks before walking into Northern Illinois University, killing six people and wounding 21, with three pistols (one chambered in 9mm and two in .380 ACP) and a shotgun. Kazmierczak had stopped taking the antidepressant “because it made him feel like a zombie.”
- 2009: Two weeks after starting Lexapro, Robert Stewart walked into his estranged wife’s work at Pinelake Health and Rehab, and opened fire. He killed eight elderly patients and wounded three others. He doesn’t remember the incident.
- 2012: James Holmes, also known as the Batman Movie killer, was taking sertraline when he walked into the showing of The Dark Knight with two .40 caliber pistols, an AR-style .223 rifle, and a 12 gauge shotgun, killing 12 people and injuring 70 others. In his personal notebook, which he sent to his psychiatrist the same day as the shooting, shows that as the medication decreased his anxiety, he lost his fear of consequences. As the dosage became higher, his thoughts became more obsessive and psychotic.
- 2013: At the time of the Washington Navy Yard shooting, Aaron Alexis was a civilian contractor working at the yard and was prescribed trazodone, a serotonin antagonist and reuptake inhibitor (SARI) that works much like an SSRI to increase serotonin levels in the brain. He killed 12 people and injured eight others.
- 2014: Ivan Lopez was a 34-year-old U.S. soldier who shot 15 of his comrades, killing three of them, at his base in Fort Hood, Texas. He was undergoing mental health treatment through the Veterans’ Administration, which is known for over-prescribing medication. The VA confirmed that Lopez was taking antidepressants (the VA only uses SSRI antidepressants) during the time of the shooting and his subsequent suicide.
- 2015: From the moment it occurred, the Charleston Church shooting has been deemed an act of white supremacy, a race crime against blacks. But two years after Dylann Roof shot and killed nine people and injured another, the court released documents that show it was more mental health than hatred that led to the murders. The documents confirmed he was taking antidepressants.
- 2016: Arcan Cetin, who was just 20 years old, walked into the Cascade Mall where he shot and killed four women, one just a teen, and shot one man, who later died at the hospital. Records show that Cetin was under the care of a psychiatrist and taking medication for depression and ADHD, including Prozac.
The list goes on and on. And with the implication of patient privacy laws, getting information on the medication and mental health diagnoses of people has become harder and harder, even with mounting evidence that there’s a connection between SSRI use and violence.
In 1996, the Health Insurance Portability and Accountability Act commonly referred to as HIPAA, was set in place. HIPAA represents the U.S.’s first attempt at national regulations for the use and disclosure of a person’s personal health information, or PHI. HIPAA makes it more difficult for medical personnel to release information regarding a person’s medical care, diagnosis, and prescription drugs, including those involved with mental health related crimes.
For example, in the 2008 Virginia Tech shooting, perpetrator Seung Hui Cho had multiple interactions with the mental health department on campus, some for suicidal ideation, but yet his parents nor authorities were never notified. University officials stated privacy laws restricted them from sharing the information.
Beyond the necessity for communication prior to these horrific shootings, after the incident, the person’s records are often protected. Even in situations where the perpetrator dies during the shooting, HIPAA protects their records for 50 years.
Because of this, the American public doesn’t know what kind of medications these people were taking and if it may have had an affect on their actions. Just looking at public shootings over the last five years, there’s a huge list of murderers who were likely on SSRIs. Here are a few:
- Zephen Xaver and the SunTrust Bank shooting
- Ian David Long and the Thousand Oaks Nightclub shooting
- Travis Reinking and the Waffle House shooting
- Nikolas Cruz and the Parkland, Florida school shooting
- Devin Patrick Kelley and the Texas church shooting
The Push for Stronger Mental Health Legislation
 With the media’s coverage of mass shootings, more and more legislation arises limiting the rights of those with mental health issues. While no one wants firearms in the hands of the mentally ill, the lack of clear language surrounding mental illness, and the limitations caused by government red tape, make knee-jerk mental health legislation dangerous and lay a path for more government control.
With the media’s coverage of mass shootings, more and more legislation arises limiting the rights of those with mental health issues. While no one wants firearms in the hands of the mentally ill, the lack of clear language surrounding mental illness, and the limitations caused by government red tape, make knee-jerk mental health legislation dangerous and lay a path for more government control.
In general, people with mental illness are rarely violent to other people. Many mental health experts and advocates agree that policies that focus on the violence of mental illness make scapegoats of the individuals, who are likely to never act violently against another person.
What’s more, according to the MacArthur Violence Risk Assessment Study (MVRAS), substance abuse was significantly more responsible for violence committed by discharged psychiatric patients than their mental health. Those patients who didn’t abuse drugs or alcohol showed no higher risk for violence than the others in their communities without mental health issues.
Laws are being created that don’t focus on the research, but on the fear of guns, thinking that stricter gun laws will keep people safer.
Red flag laws are the newest gun legislation making their way through Congress. Considered a “protective order,” red flag laws will allow a family member or law officer to petition a temporary seize on someone’s firearms if they’re deemed a threat. What a “threat” consists of isn’t clearly defined.
There’s also a push for universal background checks on all gun sales, even those sold between private individuals, and the FixNICS campaign. The philosophy behind FixNICS is that the background check system can only be as strong as the records it contains. And it’s currently missing a lot, especially when it comes to mental health issues and domestic violence.
For instance, documentation of an individual diagnosed as “mental defective,” having been involuntarily committed to a mental health setting, or having engaged in domestic abuse disqualifies that person from purchasing or owning a firearm. When this information is present in the NICS, it flags the background check and stops the sale of the firearm. But too many of these records are missing.
That was the case with the 2017 Sutherlands Springs church shooting. The gunman Devin Patrick Kelley was prohibited from purchasing firearms due to a 2012 court martial for two counts of domestic abuse. The U.S. Air Force failed to provide this information to the NICS, allowing Kelley to erroneously pass his background check and to purchase an AR-style 5.56 rifle – which he used to kill 26 people and injure 20 more. He was confronted and pursued by a neighbor, another good guy with a gun.
Gun Control, Mental Health, and SSRIs: What’s the Solution?
When it comes to mass shootings, there’s no easy solution. Violence, especially random violence, is a complex manifestation of various thoughts, feelings, and external factors. While it may be impossible to fully stop mass murders, ignoring the fact that certain medications, including SSRIs, play a role in a high percentage of these violent acts, no justice is being served.
Gun control is obviously not the solution, as the rate of mass shootings has increased over the last 30 years, at a time when multiple gun control laws have been implemented. Taking firearms away from law abiding citizens has not and will not stop the problem.
Personal Responsibility
Instead, doctors need to educate patients and make them aware of the risks, as well as take the time to explain warning signs to loved ones. If patients are taking medication for a mental health disorder, including depression, then they should see a mental health professional and be involved in mental health treatment. After all, medication – even mental health medication – does nothing to fix the problem, it only masks the symptoms.
Patients need to take some responsibility for their lives, improving their health before reaching for a mind-altering pill to make them feel good about themselves. A healthy diet, physical activity, and time spent in nature are ways to boost the mood that can help relieve the symptoms of mild depression.
The FDA-Big Pharma Connection
Lastly, the government and big pharmaceutical companies need to be held accountable for not sharing what they know about the medications they create. A study published in The New England Journal of Medicine (NEJM) looked at drug company sponsored clinical trials on antidepressants.
Of the 74 FDA-registered trials the study looked at, 38 had positive outcomes, 36 had negative outcomes. Thirty-seven of the positive outcome trials were published, but of the 36 negative outcomes trials, 22 were not published and 11 were written in a way that initially presented the data to convey a misleading positive outcome. Only three were published with unbiased and accurate information about the drug.
With this type of misrepresentation of clinical trials on medications, particularly antidepressants, the medical community and the public can’t trust medical literature for honest and reliable drug information, nor the government agency that’s designed to monitor new pharmaceuticals for safety. When medical professionals can not rely on the FDA to provide unbiased and honest clinical trial information, a true risk-benefit ratio can’t be determined and patients suffer the consequences.
Political Influence of Big Pharma
 The connection between the FDA and big pharma goes beyond clinical studies. Drug companies lure FDA employees to sit on their regulatory boards. They hire their spouses. These pharmaceutical giants utilize the field’s leading experts, who happen to be the same experts who are invited by the FDA to sit on screening panels.
The connection between the FDA and big pharma goes beyond clinical studies. Drug companies lure FDA employees to sit on their regulatory boards. They hire their spouses. These pharmaceutical giants utilize the field’s leading experts, who happen to be the same experts who are invited by the FDA to sit on screening panels.
Big pharma’s influence over the FDA goes even deeper. Drug companies spend billions of dollars on political lobbying and campaign contributions. Direct payments support the FDA budget. And in response, the FDA conceals risks and looks the other way when necessary.
The FDA also gives its own kickback to the drug companies. Only FDA-approved medications can be prescribed for government health insurance programs like Medicare, Medicaid, and through the VA. And to ensure Big Pharma continues to sell its drugs, the federal program only allows treatment claims on FDA-approved drugs.
The FDA Approval Process
The FDA approval process is a laborious and expensive endeavor, which typically takes more than a year and can cost up to a million dollars to complete. The process allows drug companies to patent their product. But when it comes to natural supplements, they can’t be patented, and therefore don’t go through the FDA approval process. Therefore supplements, which are often highly effective with little to no side effects, can not claim to “treat” a condition, even when there’s research that supports that claim.
On the surface, this may not seem like too big of a deal, but let’s circle back to Prozac, which hit the market in 1988. In the fall of 1989, the FDA recalled the supplement L-tryptophan, an amino acid that’s a precursor for serotonin and highly effective in treating depression. The recall occurred after one supplement company had an additive that caused a flu-like reaction. On March 22, 1990, the FDA issued a complete ban of L-tryptophan for public sale. Four days later, on March 26, 1990, Prozac was featured on the cover of Newsweek, along with a lead article about its benefits.
In 2001, the ban on L-tryptophan was lifted and since, research has shown it has huge therapeutic potential in the treatment of pain, insomnia, depression, seasonal affective disorder (SAD), bulimia, premenstrual dysphoric disorder (PMDD), attention disorders, sleep disorders, and chronic fatigue.
A quick note about PMDD. Premenstrual dysphoric disorder is a severe form of premenstrual syndrome, otherwise known as PMS. It officially became a medical condition in 2013 with the newest addition of the DSM-V. Yet in July of 2000, the FDA approved a new medication from Eli Lilly, the same pharmaceutical company that created Prozac. The drug was Sarafem and it was marketed to treat PMDD, which technically wasn’t even a fully recognized medical condition at the time.
Sarafem is, quite literally, the exact same medication as Prozac, only in a different color capsule. Why would Eli Lilly issue the exact same drug under a different name? It just so happens that the patent for Prozac expired in August of 2001, which allowed generic versions to be made. Eli Lilly changed the medication’s name, indicated it for this “new” disease, and the company had a new patent for Sarafem that would last until 2007.
Situations like this demonstrate that the more aspects the government controls, the worse this corruption and mismanagement becomes. Federal agencies in the hands of big pharmaceutical companies, and politicians using gun control to give a false hope to the American people, distracts them from the real cause of the current state of the nation and the frequency of mass shootings.
It’s time to personally explore the evidence surrounding the issues and come to your own conclusions.
This article first appeared at Ammo.com.
Be Free and Independent! Get a free issue of Counter Markets today.

Be the first to comment on "Prescription For Violence: The Corresponding Rise of Antidepressants, SSRIs & Mass Shootings"